The Missing Chapter in the Brochure on the “Pink Promises”
The Adult Psychiatric Department at Diakonhjemmet Hospital, Vinderen, officially defines itself as an institution providing specialized and comprehensive mental healthcare, fully committed to patient rights and high medical quality standards. According to their official statements, the department ensures:
Accurate assessment and diagnosis for each patient, using multiple scientific and methodological approaches to ensure the correct diagnosis for each individual’s situation.
Comprehensive and integrated treatment, including psychological support, medication, and involvement of a multidisciplinary team (doctors, psychologists, nurses, social workers) to ensure balanced and continuous care.
Full transparency and patient rights, including access to medical records, knowledge of what is written about them, and active participation in all treatment decisions.
Priority for patient safety and human dignity, in a safe, supportive, and non-discriminatory environment, regardless of social or cultural background.
Community support and ongoing rehabilitation, including reintegration into society, work, and family, to ensure long-term stability.
All these official promises create the impression of an ideal institution that adheres to laws and ethical standards and aims to make psychiatry a safe and healing space.
However, internal investigations and documents, including witness testimonies and audit reports, reveal that actual practices involve systematic intimidation and punitive measures, particularly targeting patients with a foreign background, and that the institution itself has been used as a tool to pressure citizens and critical journalists.
These abuses demonstrate a clear gap between the announced promises and actual practices, showing how a department meant to provide care can become a vehicle for threats and coercion, far from the medical and humanitarian goals publicly stated, in violation of national and international standards for patient rights and medical ethics.
A Psychiatric Process Characterized by Retaliation: How System Critics Become Targets in an Administrative Power Play
Within the environment of Diakonhjemmet Hospital, Adult Psychiatric Department, Vinderen, an institution expected to uphold high professional standards and medical integrity, documented records, internal assessments, and direct witness accounts reveal a complex picture of professional errors, conflicting evaluations, and structural conflicts of interest.
The documented events cannot be seen as isolated mistakes but point to a broader pattern raising questions about how psychiatric authority can be misused when institutions face criticism or accountability. The overall picture does not indicate an individual error or an isolated incident but rather a troubling example of how psychiatric power can be abused when institutions are confronted with uncomfortable disclosures or systemic criticism. In such situations, psychiatry can transform from a therapeutic practice into an administrative and disciplinary tool directed at the affected individual (the journalist).
This pattern poses risks not only to journalists but also to politicians, whistleblowers, social commentators, and others in critical roles. A system designed to protect individuals, when misused, can become a means to silence them.
In this specific case, psychiatric procedures were not used to achieve a genuine medical clarification.
A 13-Page Document with a Clear Retaliatory Tone
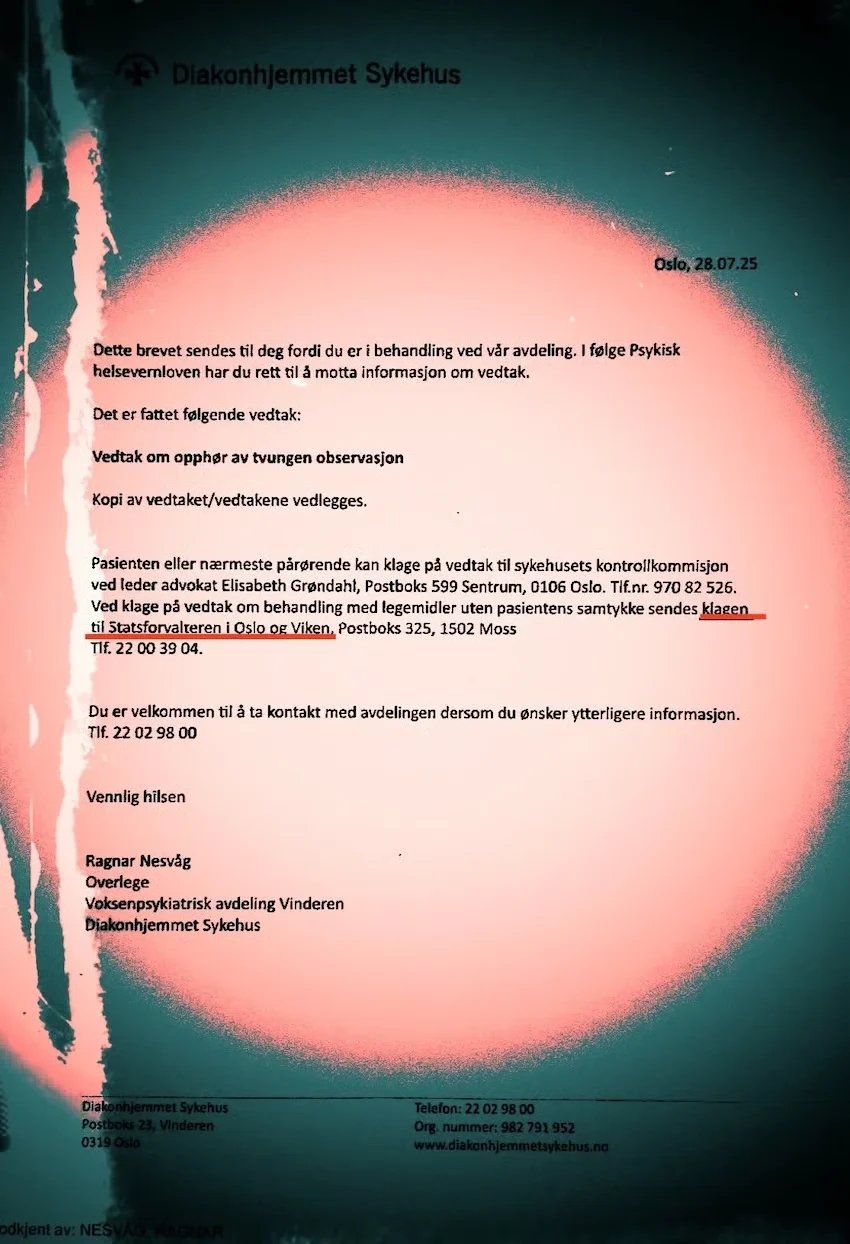
Marcus Gabrielsen and Ragnar Nesvåg prepared a 13-page assessment, a clearly punitive and repressive report dated July 28, 2025. The document was produced in just a few hours, without methodological investigation, objective testing, or comprehensive clinical examination, and therefore does not reflect a real medical assessment.
Despite this, the evaluation contained claims attempting to link the journalist’s work to an alleged psychotic condition—a classic feature of punitive psychiatry. The complete lack of professional basis, combined with the extremely limited timeframe and absence of clinical substance, underscores that the report was not intended as a legitimate medical evaluation but as a deliberate administrative and disciplinary measure to intimidate and punish the individual.
Actual Medical Findings vs. Claims
The reports simultaneously contain multiple medical statements that directly contradict the conclusions:
“No hallucinations”
“No formal thought disorders”
“Explains himself logically and coherently”
“No part of his story is impossible or can be disproven” (ref. Gabrielsen, 27.07.25)
Linking Journalistic Activity to Mental Illness
The report references his activities and journalistic posts, which are then attacked and treated as evidence of “obsession” or “paranoia.”
Blogs
Website
Pursuit of exposing corruption (as a fabricated allegation used to frame journalistic activity within a pathological narrative).
These activities are presented as evidence of “obsession” or “paranoia.” This connection completely undermines the medical narrative, as it treats freedom of expression and journalistic activity as a sign of illness, falling squarely under punitive psychiatry.
Conclusion and Legal Weakness
Despite the medical documentation, the individual was placed under involuntary observation, based on a legally weak standard formulation:
“Preponderance of probability for severe mental disorder”
Even though the document itself undermines this assumption, the legal mechanism was used to justify the coercive measure.
Testified on 01 December 2025
Doctors Marcus Gabrielsen and Ragnar Nesvåg prepared medical reports containing serious breaches of Norwegian law concerning the rights of the affected individual and mental health. The reports displayed unjustified bias, racist insinuations, and professionally unfounded claims, in addition to violations of privacy through the disclosure of personal information irrelevant to the patient’s medical condition.
The individual was transferred from the emergency department to the psychiatric institution under sedation, under unclear circumstances, despite having refused admission and lacking trust in the institution.
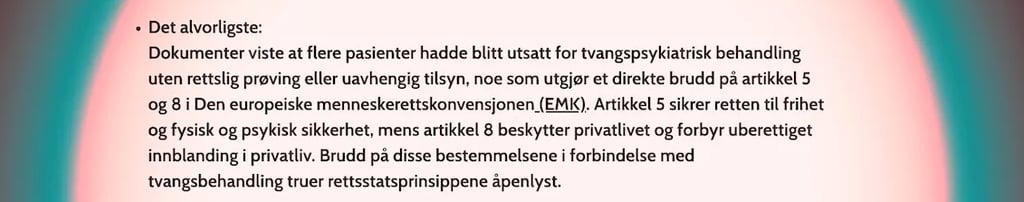
The transfer and measures took place after the individual published investigations documenting irregularities in the healthcare system, raising questions about possible retaliatory motives and compliance with Norwegian legal and professional standards, including Articles 5 and 8 of the European Convention on Human Rights, concerning the right to liberty, physical and mental security, and protection of private life against unjustified interference.
Manipulation of Medical Records: A Serious Breach of the Health Personnel Act
The individual was informed that his medical records were “blocked,” but subsequent documentation shows that the records had been accessed for several years without consent. This represents possible violations of:
The Health Personnel Act §§ 21, 25, 26
The Patient and User Rights Act (regarding access and blocking)
Access control regulations in the Health Platform (Helseplattformen)
This dual handling using the records while simultaneously claiming they were blocked, appears as an administrative maneuver to create a consistent, but artificial, background to justify the coercive measures.
Timeline Between 03:00 and 11:00: A Systematic Regime of Pressure
Between 03:00 and 11:00, the individual was held in an emergency room without food, water, or the opportunity to assert his rights. According to documentation, he was:
Non-aggressive
Cooperative
Logical and oriented
Able to recount his history coherently
Yet, coercive measures were implemented.
Nesvåg subsequently drafted a parallel report with a medical student, which largely mirrored Gabrielsen’s first assessment, a clear sign of documentary harmonization to support a predetermined action.
Unethical Suspicion and Reuse of Legally Rejected Claims
The psychiatric assessments used previous accusations formally dismissed or legally rejected. Despite having no legal or factual value, these were reused in the reports as alleged “risk markers.”
The report authors also attempted to contact the police and other authorities who had escalated the conflict to identify a case against the journalist. All attempts failed, and the police confirmed there was no registered case or circumstance justifying involuntary hospitalization.
Using legally rejected claims and seeking external support demonstrates that the purpose was not medical assessment or treatment, but a retaliatory administrative measure to portray the journalist as a fabricated “risk.”
This becomes especially evident with the role of doctor, who used the term “potential danger” as a tool of coercion. He had previously criticized patients collectively, labeled them unreliable and dishonest, and expressed contempt for the complaint system at the County Governor’s Office in Oslo. “Potential danger” was thus used to create artificial internal fear and mobilize staff in support of the measures, particularly after audio recordings revealed multiple breaches of health law.
“Potential danger” was transformed from a precise medical criterion into an administrative pretext serving a predetermined goal unrelated to medical or psychiatric assessment, but aimed at silencing a journalist exposing internal misconduct.
Alleged Imovane Intake / Medical Improbability and Lack of Testing
The individual claimed to have taken 30 mg of Imovane before arrival at the emergency room. However:
No toxicology tests were conducted
No measurements support the claim
Observations show he walked independently, interacted with nurses and Dr. Marie Veland, and was oriented and not somnolent
After meeting with Veland, he was transported in a state consistent with pharmacological sedation, arriving at the psychiatric unit in a wheelchair and later described as “very sleepy.”
Pharmacologically, a patient cannot:
Be fully oriented and speak normally at the emergency room
Then become suddenly deeply somnolent
And awaken lightly shortly after arrival at the psychiatric unit
This pattern does not correspond to hypnotics like zopiclone (Imovane), but is consistent with procedural sedation after triage.
Documentation Gaps and Denial of Access
The individual arrived walking, awake, and cooperative, but was later transported in a wheelchair, unconscious.
No notes or analyses support that he had self, administered sleep medication
No pills were found
Several nurses documented he was able to speak and explain his health and social situation
Claims of a long psychological interview are false; the meeting lasted only minutes, with guards outside the room
He confronted emergency room leader Katia Monclair, who initially admitted a need for investigation and correction of the records but withdrew after “higher, level intervention.”
The emergency department refused access to surveillance videos and audio recordings documenting the nurse’s request for him to appear at the emergency room.
All of this occurred over more than five hours, at a time with no witnesses or other patients present.
Conclusion: Forced medication, denial of access to evidence, and rewriting of facts indicate illegal involuntary hospitalization disguised as healthcare, not a legitimate medical assessment.
A Diagnostic Collapse F22 in Just 9 Hours
The individual:
Admitted at 03:00
Assessed at 09:00
Received F22 (paranoid psychosis) within 9 hours
Diagnosis was revoked the same day
This shocking timeline, documented in official Diakonhjemmet Hospital records under the signatures of Marcus Gabrielsen and Ragnar Nesvåg, violates professional psychiatric standards and clearly shows the diagnosis was used as:
A tool of fear and control
A basis for coercion and confinement
Not as an objective medical evaluation
Everything indicates the diagnosis was used as an authoritarian instrument to justify restrictions and enforce compliance, not to safeguard health.
Internal Contradictions, A Revealing Quote
From Gabrielsen’s professional assessment:
“No part of his story is impossible or can be disproven.”
This alone undermines the entire basis for an F22 diagnosis, which relies on delusional content.
Conclusion: A Structural Problem, Not an Individual Decision
This case reveals a practice consistent with “punitive psychiatry”, where psychiatric structures are used to discipline system critics.
The individual was:
Oriented
Logical
Non-hallucinatory
Non-violent
The case tests not only the professional competence of psychiatry at Diakonhjemmet Hospital, Vinderen DPS, but also the credibility of the healthcare system in Oslo, and its capacity to withstand criticism without using medical authority as a tool for domination.
There is an alarming trend in Oslo, where medical practices have begun shifting toward extremism: psychiatry is used to intimidate and control, rather than treat. Old accusations are reused as risk markers, records are blocked, and the system’s integrity is at risk. Psychiatry risks losing its role as a safe refuge for patients and instead becoming an administrative instrument undermining fundamental human rights.
Critical Questions: Is psychiatry in Oslo at risk of being used as a tool of power and domination over individuals, silencing journalists, suppressing freedom of expression, and obstructing accountability mechanisms, rather than serving as a therapeutic and preventative institution? This development threatens the integrity of the healthcare system and its role as a safe haven.













Marcus Gabrielsen
Psykiater
Ragnar Nesvåg
Psykiater
"Message received!"
Morning of July 28, 2025: Tension at the Adult Psychiatric Department, Diakonhjemmet Hospital, Vinderen
Early in the morning of July 28, 2025, an unusually tense atmosphere prevailed at the Adult Psychiatric Department of Diakonhjemmet Hospital in Vinderen, amid ongoing meetings, with the top floor functioning as an informal coordination hub.
The affected individual contacted the Patient and User Ombudsman, who immediately confirmed that there was no legal basis for continued involuntary hospitalization and demanded immediate release.
At 11:00 AM, Nesvåg informed the individual with a tense tone:
“You are free… go out now.”
However, the individual refused to leave until he could access the documents underpinning the decision.
Despite this, Nesvåg, together with his trainee, continued writing reports for several hours, filled with:
Unfounded claims and personal accusations
Derogatory insinuations, including explicitly racist undertones
No clinical examination or professional contact with the individual
The reports carried a clear political dimension, as the individual is an active journalist exposing critical irregularities in the healthcare system.
The drafting and delivery of these reports were completed at 16:40, following a series of internal meetings. The documents reflected no objective or clinical assessment; instead, they appeared as administrative tools for control and retaliation, aimed at justifying a predetermined decision and achieving personal and administrative objectives at the expense of the individual’s rights and the institution’s transparency.
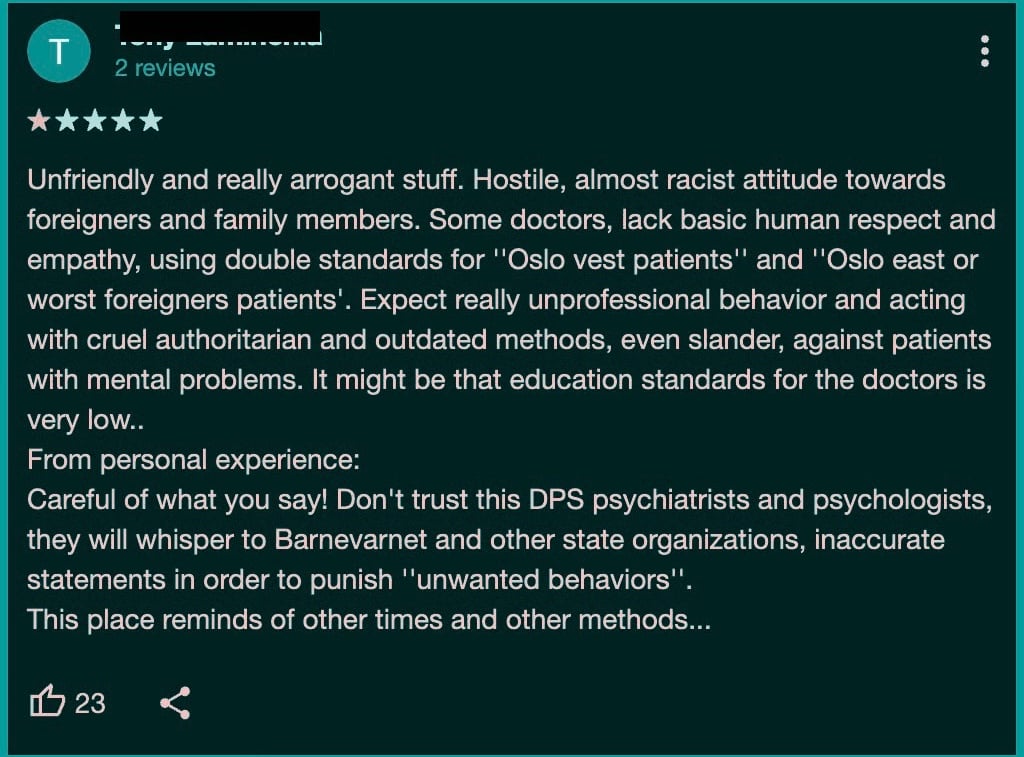
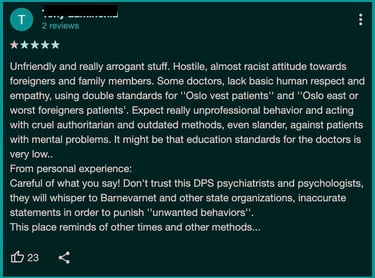














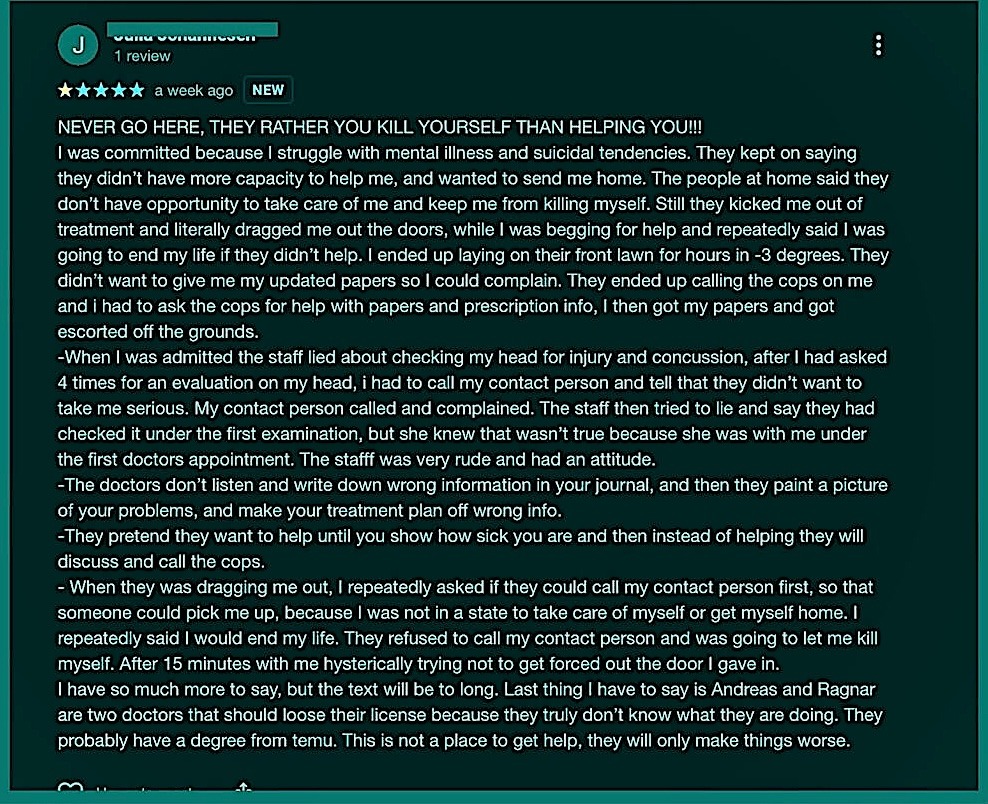
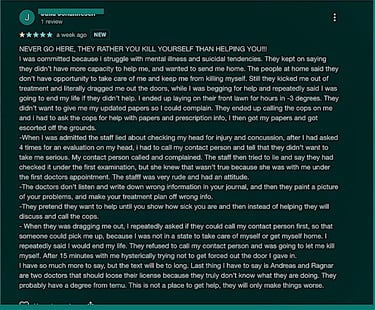
Patients’ and relatives’ experiences before the deletion of comments at the Adult Psychiatric Department (VPA) at Vinderen, Diakonhjemmet Hospital, reveal aspects of treatment that often remain hidden, and may be far more serious than expected.
Documents and witness accounts suggest that formal standards are not always upheld, and that patients’ health, rights, and dignity may be at significant risk. This includes, among other things, unlawful disclosure during the exercise of the right to file complaints. Many patients also experience stigmatization, public shaming, and humiliation, often resulting from assessments that appear biased, influenced by the practitioner’s mood, preferences, or personal concerns, and which fail to reflect the patient’s actual life situation.
Diakonhjemmet Hospital generally has a good reputation and acceptable professional standards, with structured routines and stable practices in its general departments. However, the poor reputation of the Vinderen unit remains a cold, persistent stain on the hospital, associated with the use of oppressive and arbitrary methods in patient care.
Documented experiences from the Adult Psychiatric Department at Vinderen reveal a troubling history, showing a substantial deviation from the level of care found in the rest of the hospital. Treatment here is reported to be marked by repeated violations of patients’ rights, complaints that go unanswered, and warnings that are ignored, reflecting systematic neglect and a lack of responsiveness to criticism.
This practice raises serious questions about the fate of the patients and requires immediate action to safeguard their rights and improve the quality of healthcare services.


Political abuse of psychiatry is the exploitation of psychiatric diagnoses, involuntary confinement, and treatment for oppressive purposes, aimed at obstructing the fundamental human rights of certain groups and individuals in society.
Misuse of Authority and Public Shaming by Ragnar Nesvåg
Ragnar Nesvåg insisted on sending his reports to all relevant healthcare services in a public and conspicuous manner, despite the affected individual’s explicit refusal. This action did not constitute a medical assessment, but rather served as a tool for intimidation, public humiliation, and social punishment, targeting the individual to suppress his revelations of administrative corruption documented in his publications.
Hospital management failed to respond to formal complaints, indicating a likely prearranged coordination among the involved actors and supervisory authorities, whereby patient rights and healthcare laws were disregarded.
This action represents a profound erosion of ethical standards, in which medical authority is misused as an instrument for control, revenge, and coercion. At institutions such as Aker Emergency Department and Diakonhjemmet Hospital, power was leveraged to damage an individual’s social reputation and impose punishment, far beyond any legitimate medical assessment.
The events underscore how authority can be transformed into a mechanism of injustice, and highlight that ethics are crucial for safeguarding human dignity against systematic abuse.
Statsforvalteren,klage på helse-og omsorgstjenester
Legevakten Aker i Oslo,Katja Monclair
Diakonhjemmet sykehus, Voksenpsykiatrisk avdeling Vinderen
Psykiater Ragnar Nesvåg, Psykiater Marcus Gabrielsen
Kontrollkommisjonens Elisabeth Grøndahl
Revelation: What Is Happening at Diakonhjemmet Hospital, Adult Psychiatric Department Vinderen
Documents from the department, together with patient testimonies and lived experiences, reveal serious and ongoing unethical practices at Diakonhjemmet Hospital, Adult Psychiatric Department Vinderen. These practices constitute clear violations of medical ethics, patient rights, and fundamental human rights.
Flawed Assessments and Unprofessional Evaluations
According to available official documents, patient assessments in many cases are not based on objective medical standards. Numerous patients have been subjected to incorrect and unprofessional classifications grounded in personal impressions or social and cultural bias, without support from documented medical evidence. These assessments have caused severe harm to patients’ reputations and have damaged their psychological, social, and legal lives, particularly when driven by conscious prejudice or stereotyping.
Violation of Privacy
One of the most serious practices involves the recording of highly sensitive personal information about patients’ private lives, including details about romantic relationships, names of partners, doubts about their ability to care for their children, and even questioning their humanity and basic life skills. This information is not used for therapeutic purposes but instead functions as a weapon to undermine patients socially and legally. In several cases, harmful medical reports were deliberately sent to general practitioners, family members, or outdated addresses where patients no longer lived, exposing private information to unrelated third parties and significantly worsening patients’ psychological and social distress.
Unacceptable Practices
These practices go far beyond legitimate clinical observation and include excessive surveillance of body language, speech, clothing, walking patterns, and even how often patients use the restroom. Such observations are later interpreted arbitrarily as symptoms or accusations. This surveillance is frequently filtered through cultural or ethnic stereotypes, representing a clear violation of patients’ fundamental rights and professional medical standards.
Linguistic Stigmatization and Racialized Terminology
A review of medical records, internal notes, and patient testimonies reveals a systematic and problematic use of the term “immigrant” in reference to patients with foreign or minority ethnic backgrounds. The term is not employed as a neutral descriptive category, but is repeatedly used in a manner that carries an implicit negative connotation and functions as a signal of deviance, lower status, or lack of belonging. In several cases, the label “immigrant” is applied even when it is medically irrelevant, and where the patient’s citizenship, length of residence in Norway, or individual life circumstances have no documented relevance to the assessment. This language use appears racialized and contributes to reducing individuals to their presumed ethnic origin, while simultaneously legitimizing stereotypical assumptions about functional capacity, credibility, and treatment needs. Such linguistic practices contribute to institutional discrimination, normalize unequal treatment, and undermine both patient dignity and the fundamental principles of equitable healthcare.
Discrimination Against Patients with Immigrant Backgrounds
Documented information and patient experiences indicate that admission to the department often occurs on a selective basis, where some patients are granted access while others are excluded, leaving them without necessary treatment, which exacerbates their health and social conditions. Repeated reports reveal a pattern of systematic discriminatory treatment against patients with an immigrant background, and even when they are admitted, foreign patients are assigned to different units without transparent or verifiable criteria. While some patients are placed in open and comfortable wards with a high degree of freedom and convenience, patients with an immigrant background are disproportionately placed in closed and restrictive units with a prison like or detention like character, negatively affecting their lives and health. Complaints and observations from these patients are often recorded negatively in their medical files and later used against them in treatment processes, further restricting their access to adequate healthcare.
According to official reports, the documents reveal a recurring pattern targeting foreign patients: when they are admitted through the emergency units and transferred to the department due to serious, and sometimes critical, conditions, they are deliberately forced to leave the department the following day, while their relatives are contacted by phone with explicit threats that if they do not come to pick up the patient, they will be transported to them by taxi. These practices indicate a systematic policy targeting foreign patients and pushing them out of the hospital, carried out to exert pressure on their families and deny them the possibility of remaining within the healthcare system in Oslo. This constitutes a clear violation of their fundamental rights to treatment and protection.
The documents show that some foreign patients were not admitted until the health authorities under the Statsforvalteren Health, Care and Social Services in Oslo intervened, demanding that the department accept them following a series of rejections and exclusions from the healthcare system, revealing an undeclared policy that discriminates against foreign patients and has led to their prior denial of necessary healthcare.
Manipulation and Obstruction of Complaints
Although patient rights legislation grants individuals the right to hold health authorities accountable, this right is routinely undermined in practice. Health authorities employ delays, administrative obstacles, and procedural complexity to prevent complaints from being fairly addressed. This prolonged process traps patients for years in cycles of distress, uncertainty, and powerlessness.
Repeated Alerts and Reports to Health Authorities
The material shows that the health authorities under the County Governor have, over extended periods, received numerous complaints and alerts regarding practices at the Adult Psychiatric Department Vinderen. These reports describe patterns of systematic mistreatment, particularly affecting patients with foreign backgrounds.
Several reports document the creation of unethical and stigmatizing medical records lacking scientific foundation, resulting in lasting social and legal harm to patients. In addition, documented concerns were raised regarding potential conflicts of interest, including information suggesting that staff members received gifts. Such circumstances raise serious questions about professional integrity, impartiality, and compliance with core ethical standards in healthcare.
Despite the seriousness and repeated nature of these alerts, the available information raises substantial doubts as to whether they were subject to genuine, independent, and effective follow up. This reinforces the impression of a system where complaints accumulate without resulting in meaningful structural change.
Manipulation and Distortion of Medical Records
One of the most severe practices involves the manipulation of original medical records as retaliation against patients who submit complaints. Reports are distorted or replaced by new documents with a punitive character, signed by senior physicians. This makes it nearly impossible to trace the original assessments, shields those responsible from accountability, and further worsens the patient’s condition.
Psychological and Social Coercion
When patients attempt to correct inaccuracies or express their suffering, they encounter institutional resistance that escalates into psychological and social coercion. This deepens feelings of helplessness and despair, trapping patients within a system that operates in direct conflict with ethical principles.
Destructive Consequences After Discharge
The consequences of these practices extend long after patients are discharged. Harmful reports follow patients to general practitioners and other institutions, damaging reputations, restricting access to future healthcare, and destabilizing family and social relationships. In some cases, such reports enable further exploitation by unethical practitioners.
Need for an Independent and Transparent Investigation
The situation at Diakonhjemmet Hospital is not the result of isolated incidents but reflects long standing unofficial practices affecting specific patient groups. This demands an independent and transparent investigation beyond the hospital’s internal structures. Such an investigation must include a thorough review of medical record handling, diagnostic practices, patient placement procedures, and complaint management systems.
Systematic Secrecy and Suppression of Criticism
These cases are managed under conditions of extensive secrecy, creating an environment of fear and limiting the possibility of truth being exposed. Evidence indicates that patient testimonies and critical comments are swiftly removed from the hospital’s online platforms, even when posted anonymously. Individuals who speak out face threats of defamation and social stigmatization, reinforcing a hostile environment that discourages victims from sharing their experiences.
Positive Contributions from Ethically Committed Staff
Despite the structural failures, there are nurses and healthcare professionals who demonstrate exceptional ethical commitment and genuine dedication to patient care. Their efforts have had a significant positive impact on patients’ lives. While this commitment is not universal, acknowledging those who uphold professional integrity remains essential within a deeply troubled system.
"The announced events provide a vivid picture, but what remains hidden is greater."
These events confirm the accuracy of previously published reports; practical experience shows that involuntary hospitalization without legal oversight or independent supervision leads to serious violations of patients’ rights and exposes the healthcare system’s failure to uphold legal and ethical standards.
Regardless of the scope of the documented material, the central analytical question is whether these findings reflect isolated procedural failures or point to a deeper institutional pattern. Given the documentation of involuntary admissions and diagnostic assessments employed beyond their therapeutic purpose, a simple enumeration of cases is insufficient. What follows is a structural analysis of the logic underpinning these practices.
The central conclusions can be summarized as follows:
The documents and accumulated testimonies show that the institution does not operate according to the principle of neutral health care, but rather according to a logic shaped by social and cultural sorting. Medical assessment does not appear to be the decisive factor in determining a patient’s course. Instead, background, language, social position, and the degree of symbolic compliance with medical authority seem to be determinative. In this way, diagnosis is transformed from a therapeutic tool into a means of classification and control.
A stable pattern of institutional discrimination against patients with foreign backgrounds becomes evident. This manifests not only at the level of language, but in concrete decisions related to admission, distribution across wards, the degree of restrictions imposed, the speed of discharge, and the handling of complaints. The repeated use of terms such as immigrant without medical relevance reveals an administrative mindset in which identity itself is treated as a risk factor.
The practice is not limited to exclusion, but extends into what can be described as concealed punishment under a therapeutic guise. Rapid and forced discharge following emergency admission, threats of forced transport, and the systematic placement of foreign patients in closed units with prison like characteristics collectively indicate the use of medical measures as tools of pressure and deterrence rather than protection.
The handling of medical information exceeds its therapeutic purpose and assumes a socially and legally harmful function. The recording of personal details without therapeutic relevance, the forwarding of damaging reports to actors outside the health care context, and the distortion of patient records contribute to turning medical documentation into a long term instrument of discipline.
Mechanisms of accountability appear, in practice, to be effectively neutralized. Delays in complaint processing, manipulation of reports, replacement of original assessments, and systematic administrative inertia create the image of an institution that prioritizes shielding itself from scrutiny over protecting patients from harm. The fact that the supervisory authority has intervened in certain cases does not weaken this assessment, but rather underscores that corrective action occurred only under external pressure.
What emerges is a long term pattern rather than situational deviations. Repetition, similarity in the course of events, and their persistence over time, combined with the absence of structural reforms, indicate the existence of an informal yet effective practice that tolerates abuses as long as they affect specific groups.
The presence of professionally competent and ethically conscious individuals within the institution does not contradict these findings, but instead highlights a fundamental paradox. Individual integrity operates here against the institutional current, not as a product of it. This confirms that the problem does not lie solely with individual actors, but within the framework in which they operate.
What these facts reveal is that we are confronted with a health institution that has partially drifted away from the logic of care and toward a logic of social control. Certain groups, particularly patients with foreign backgrounds, are not regarded as individuals entitled to equal rights, but rather as an administrative burden or as a group perceived through a security-oriented lens disguised in medical terms.
This structural deviation is reinforced through a parallel narrative produced in the public sphere, especially on social media platforms. The images and materials disseminated do not serve a documentary function; instead, they are carefully crafted to present a polished and reassuring representation of the institution and its staff, portrayed as exemplars of humanity and professionalism. This representation does not reflect reality so much as it constructs an alternative symbolic reality, the purpose of which is reputation management rather than scrutiny of practice.
The gap between this staged reality and the reality exposed by documents and testimonies is neither incidental nor innocent. It serves a clear institutional function: to dilute accountability and redirect attention, thereby allowing practices to persist that cannot withstand independent examination.
In this sense, what we are facing is not merely a therapeutic failure, but an integrated system that combines deviations in practice with distortion in representation. This places the institution in a position of serious legal and ethical accountability and renders the demand for an independent and transparent investigation an institutional necessity rather than a moral choice.
Diakonhjemmet Hospital, Adult Psychiatric Department, Vinderen
Forskningsveien 7 and 13, 0373 Oslo, Norway

Adult Psychiatric Department (Vinderen), Forskningsveien 7, 0373 Oslo
Dokumentasjonen viser at hendelsesforløpet eskalerte gjennom den aktuelle legen, som overtok kontoret til den pensjonerte legen ved Skøyen Helsesenter i 2022 og 2023. Dokumenter og vitneutsagn indikerer at hans administrative innflytelse ble brukt på en måte som skapte et klima av press og skremsel, ved å bruke enkelte helsearbeidere som redskaper for urettmessig påvirkning, etter at det dukket opp pålitelige opplysninger som stilte spørsmål ved lovligheten og sikkerheten i hans yrkesutøvelse.
Disse forholdene viser en kompleks bakgrunn som illustrerer hvordan misbruk av helsemyndighet kan bli et uetisk virkemiddel som påfører pasienter psykisk, moralsk og samfunnsmessig skade. Det har blitt rapportert om forsøk på å stigmatisere enkelte pasienter med psykiske betegnelser som ikke var basert på korrekte medisinske vurderinger, samt utarbeidelse av rapporter med straffende eller sjikanerende karakter, som fremstår som reaksjoner på at pasientene uttrykte fakta eller informasjon som ikke ble ønsket av enkelte ansvarlige.
Dokumentasjonen viser også bevisste forsøk på å true og stilne journalister og kritikere som avslørte eller dokumenterte overgrepene, inkludert implisitte trusler og press for å hindre publisering og undersøkelser, med mål om å hindre sannhetens fremkomst og beskytte visse myndigheters interesser.
Dokumentasjonen av denne saken reiser også spørsmål om lik anvendelse av lovverket i Oslo, spesielt overfor pasienter med utenlandsk bakgrunn, der det rapporteres om forskjellsbehandling som undergraver deres rettigheter og menneskelige verdighet. Dette viser et potensielt mønster der enkelte borgere ikke blir anerkjent som fulle rettssubjekter, til tross for at de har de samme juridiske rettigheter som andre, slik grunnloven fastslår når det gjelder likhet og beskyttelse av alle borgeres grunnleggende rettigheter.
Denne helheten reiser grunnleggende spørsmål om prosedyrsikkerhet, rettssikkerhet og skillet mellom medisinsk myndighet og individets rettigheter, og understreker behovet for en uavhengig gjennomgang for å sikre at helseinstitusjoner ikke blir brukt i praksiser utenfor sitt profesjonelle og humanitære rammeverk i Oslo.